School Intervention with Recreational Motor Activity for Overweight Children
Gabriela de Oliveira
Henrique Flore Cavenago
Tamara Beres Lederer Goldberg
Emerson José Venancio
Altamir dos Santos Teixeira
Carla Cristiane da Silva
*Corresponding author: Carla Cristiane da Silva ccsilva@uel.br
Cite this article
Oliveira, G., Cavenago, H.F., Goldberg, T.B.L., Venancio, E.J., Teixeira, A.S., & Silva, C.C. (2022). School intervention with recreational motor activity for overweight children. Apunts Educación Física y Deportes, 147, 17-25. https://doi.org/10.5672/apunts.2014-0983.es.(2022/1).147.02
Abstract
The objective of this study was to verify the effect of a 12-week school intervention with recreational motor skills on parameters of body weight control, motor competence, and physical fitness in overweight students. The sample included 26 overweight children evaluated before and after a 12-week intervention period with recreational activities. Total body mass, height, abdominal circumference, skinfolds, physical fitness, and motor competence tests were collected. Results showed that recreational physical training significantly impacted on relative body fat reduction (pre = 28.3%; post = 26.1%, p = .03) and abdominal adiposity (pre = 71.0 cm; post = 68.1 cm, p = .04). A positive effect was observed on motor quotient, derived from better motor competence. The recreational physical training program was effective in reducing global and abdominal adiposity, as well as facilitating significant increases in motor competence, and cardiorespiratory and muscle physical fitness.
Introduction
Child and youth obesity has increased worldwide, and in Brazil the prevalence is approximately 15% in children and teenagers between 2 and 19 years of age (Aiello et al., 2015). Obesity is known as a chronic disease of pediatric origin, and although some clinical outcomes manifest at early ages, others appear with higher intensity in adult individuals (Mosca et al., 2017; Nemet, 2018). During childhood, obesity has a negative impact on physical, social, and emotional health, and self-esteem. Overweight children have 17% to 30 % more chances of suffering bullying compared to normal weight children (Reulbach et al., 2013). At school, discrimination occurs in the form of verbal aggression, threats, and exclusion from groups (Bacchini et al., 2015).
In addition to these negative psychosocial implications, obesity leads to lower motor competence levels, which generates concomitant low levels of habitual physical activity in a cycle with negative feedback (Henrique et al., 2020; Sentalin et al., 2019). Thus, a systematic review study found evidence that excess body weight is associated with lower levels of motor competence, as well as a higher probability of giving up physical activity in childhood, and this inactive behavior can last during youth and adulthood (Cattuzzo et al., 2016). Valentini et al., 2020 highlighted that motor competence was a significant predictor of the level of habitual physical activity, where children with greater motor competence engaged more actively in Physical Education classes. On the other hand, heavier children perceived themselves as less competent in physical tasks and social interactions (Valentini et al., 2020; Stodden et al., 2008).
In contrast, training in fundamental motor skills for kindergarten students, instructed by a specialized professional, three times a week, improved motor proficiency and increased the intensity of habitual physical activity. As a consequence, sedentary behavior decreased together with a reduction in childhood obesity (Engel et al., 2018). In short, children with good motor coordination are more predisposed to engage in sports activities (Vandorpe et al., 2012). Confirming these findings, a sequential study of 27 years attested that the habitual physical activity level around the age of 6, significantly predicts physical activity in youth and adulthood (Telama et al., 2014), demonstrating that development of physical activity at pediatric ages can be stable and long lasting.
However, although the positive impact of motor practice in childhood on body weight control outcomes is recognized, it is known that the quality of available environmental stimuli for children is not enough to develop motor competence. Recently, researchers stated that physical education classes are commonly overcrowded, and the available space for physical activities is restricted both at school and in the community (Ré et al., 2018). Moreover, it was reported that children spend more time on sedentary behavior during the school term (Da Costa et al., 2017), and for this reason, it is important to introduce active breaks in all school disciplines, in order to reduce sedentary behavior time (Brusseau et al., 2018; Carlson et al., 2015). Thus, the need to intervene in school physical education classes is recognized, since students, especially obese students, need well-structured activities, intense enough to control body weight and other health-related variables (Bravo et al., 2020). Furthermore, improvement in children’s physical fitness can have a remarkable influence on the quality of physical and mental health (Gu et al., 2016), as well as leading to a healthier lifestyle (Kari et al., 2016; Yuksel et al., 2020).
Accordingly, priority should be given to intervention strategies that increase physical activity and motor competence levels, mainly in kindergarten and elementary students (Ré et al., 2018). Recently, a Spanish study observed a low motor coefficient in 37.5% of preschoolers who participated exclusively in Physical Education classes. The authors considered that the short period of time in classes dedicated to motricity explains the low motor development observed among preschoolers (García-Marín & Fernández-López, 2020). Similarly, in Brazil, a cross-sectional study identified that children between 3 and 5 years of age who play sports in addition to school physical education classes present significant advantages in motor competence over non practicing children (Queiroz et al., 2014). Another Brazilian investigation observed that higher levels of locomotor skills in children of preschool age are associated with a lower risk of obesity, and that participation in sports that stimulate these skills are fundamental for individuals to engage in sports practice in early childhood (Henrique et al., 2020, 2016). In this scenario, it seems mandatory to incorporate additional extra-curricular practices into Physical Education classes to achieve adequate levels of motor competence, physical fitness, and weight control in childhood.
Based on these assumptions, the objective of the current study was to verify the effects of a school intervention with recreational motor skills during 12 weeks on parameters of body weight control, motor competence, and physical fitness in overweight students.
Methodology
Materials and methods
The study has a quasi-experimental design (pre/post test) with a sample selected by convenience due to the exploratory nature of the study. In total, 26 students of both sexes were included, aged between 6 and 9 years of age, 13 female and 13 male. The study received previous approval from the Human Research Ethics Committee (CAAE: 62267516.2.0000.5231).
The eligibility criterion for the included children was a Body Mass Index (BMI) above the 85th percentile, i.e. classified as overweight according to the Centers for Disease Control and Prevention criteria (Kuczmarski, 2002). Children undergoing nutritional monitoring or already included in a regular physical activity program, other than usual physical education classes, were excluded from the data analysis. The children’s routine was not changed concerning eating habits, with only the addition of scheduled sessions of recreational motor activities. Furthermore, the predictive equations of Slaughter et al. (1988) were used for information on relative fat, to measure the triceps and subscapular skinfolds.
To ensure that all children included were in prepubertal or early puberty stages, skeletal maturation was assessed using hand and wrist radiography to obtain bone age, using the Greulich & Pyle method (1959). The exams were documented by a radiologist with extensive experience (blind evaluator).
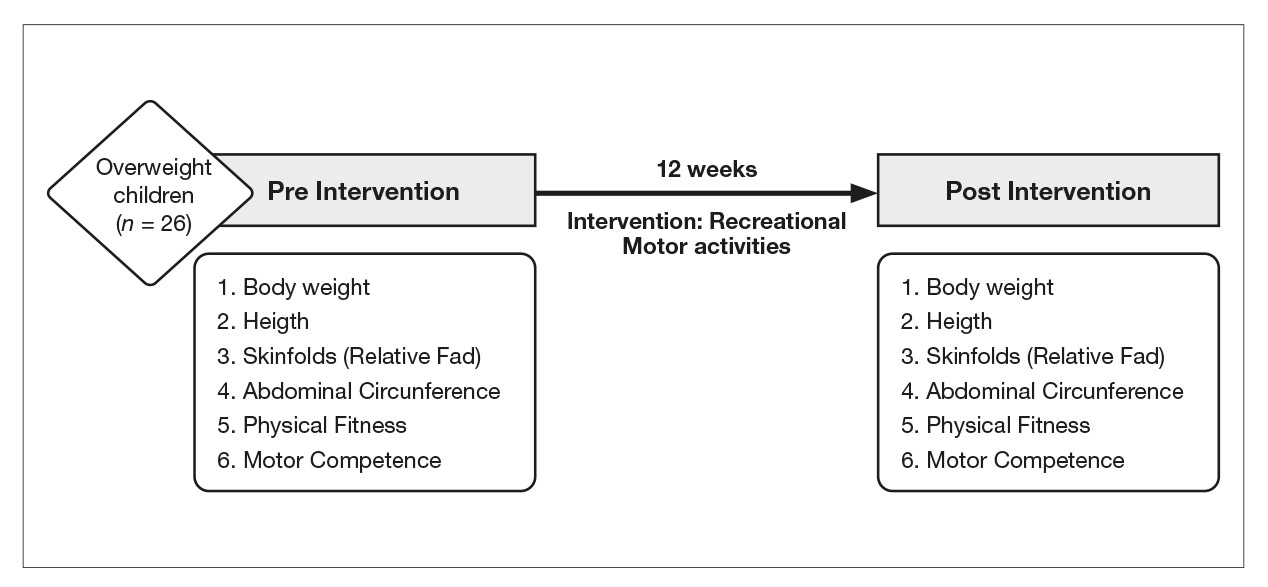
Flowchart 1 highlights the stages of the study and the moments of assessment before and after 12 weeks of intervention with recreational motor activities.
All participants studied at the same full-time school and performed the intervention for 12 weeks during the extra-curricular period, totaling 36 sessions. The intervention took place three times a week on alternate days, lasting 60 minutes per session. Sessions were organized involving children in intermittent locomotor activities (running, jumping, moving); manipulation with balls (kicks, throws, tumbling), and stabilization (dynamic balance), all of which are recreational and collective, in order to ensure motivation for the practice (Errisuriz et al., 2018). The activities were carried out in a combined way so that the children performed activities of play, recreational games (catches, relay races, circuits), and dance. The internal training load was measured using a Polar® RS800, (Kempele, Finland) heart rate monitor. The intensity of the sessions reached a minimum of 70% of the maximum heart rate previously calculated by a specific predictive equation for pediatric groups (Mahon et al., 2010). The weekly frequency of intervention sessions was arranged using a roll call.
In order to verify the effect of the intervention on motor competence parameters, the Test of Gross Motor Development (TGMD2) was used, proposed by Ulrich (2000), and posteriorly validated for the Brazilian population (Valentini, et al., 2012). The tests are composed of 12 motor skills, six for locomotion (running, canter, one-legged jump, obstacle hop, horizontal jump, and side run) and the other six for object control skills (hit, bounce, receive, kick, throw over the shoulder, and roll). In order to assess these skills, an experienced and trained evaluator demonstrated every movement and then the students tried once. During this trial attempt, the evaluator observed if the individual understood the move properly, and if not, a new demonstration was given. The students were filmed during two attempts at each skill which were then checked against the test scoring criteria, through completion of a specific registration form by three independent and experienced appraisers. The analysis of the motor competence videos was performed blindly, without contact and/or confirmation of the results by the evaluators.

For the outcome of physical fitness, the battery of motor tests of the Projeto Esporte Brasil (PROESP) was used (Gaya & Gaya, 2016). Cardiorespiratory fitness was investigated by the six-minute running test; the abdominal test was performed to detect strength and localized resistance; and the sit-and-reach test to check flexibility levels. All tests were performed on the court, following specific execution and classification criteria. Prior to the official evaluation day, the tests were performed with all children in order to familiarize them with the motor tests. The application occurred with one experienced evaluator and an assistant. The researchers who typed and processed the statistical analysis were blinded to the data collection, analysis of motor skills, and the intervention process.
Data normality was verified using the Kolmogorov-Smirnov test, confirming a non-parametric result, followed by the application of the Wilcoxon test to identify the existence of differences between the pre and post-intervention moments. All procedures were performed using the SPSS 20.0 statistical package and a significance level of p < .05 was adopted.
Results
The results demonstrated that, before the intervention, all included children were in prepubertal or early puberty stages, with a mean bone age of 7.2 years, minimum 5.0 years and maximum 10 years. In addition, chronological age presented similar values, with a mean age of 7.7 years, minimum 5.7 years and maximum 10.1 years.
Regarding the impact of the intervention on body weight control, Table 1 shows median and interquartile range values at pre and post-intervention moments of anthropometric and growth variables. The results demonstrate a significant effect of intervention on reduction in total relative body fat and abdominal adiposity.
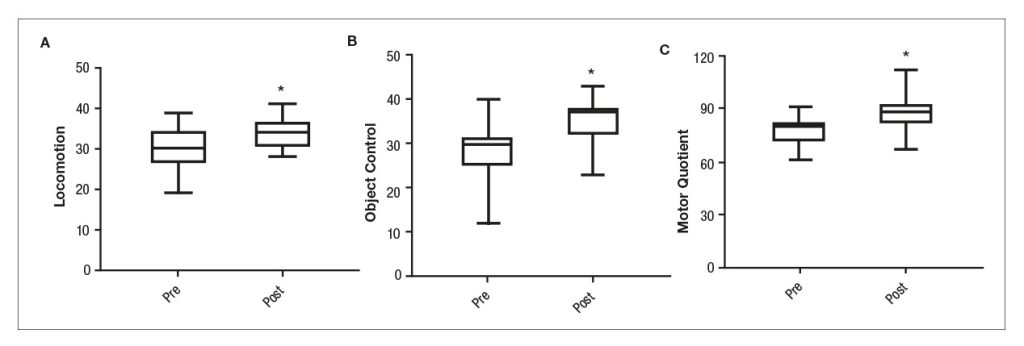
The results of the impact of the motor intervention show positive effects of 12 weeks of recreational motor activities in overweight children. There were significant improvements (p < .05) in locomotion and object control, reflecting significantly in the increase in motor quotient (median pre = 76.0 (63.2-79.7); post = 85.0 (76.0-91.0); p = .001) (Figure 2).
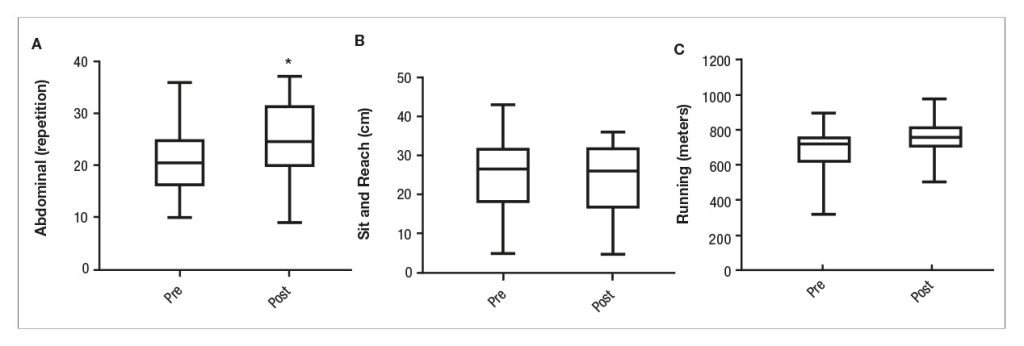
The effects on physical fitness parameters are shown in Figure 3. There was a significant increase in abdominal localized muscle resistance (median pre = 20.5 repetitions [16-25]; post = 24.5 [19.7-31.5]; p = .043) and aerobic power assessed by the running test (median pre = 720 meters [609.7-762.2]; post = 757.5 [690.7-819]; p = .015). The sit-and-reach test performed to investigate flexibility did not demonstrate any significant difference after the intervention with recreational motor activities.
Discussion
The main results of the present study indicate a significant effect on reduction in relative body fat and abdominal adiposity, in addition to improvement in motor skills for locomotion and object control, which positively reflected on the motor quotient. Regarding the variables of physical fitness, there was a significant increase in localized abdominal muscle resistance and cardiorespiratory fitness.
Similar results were observed by Delgado-Floody et al (2018), indicating that after 28 intervention weeks of High Intensity Interval Training (HIIT), with children between 6 and 11 years of age, there was a significant reduction in obesity through a reduction in the fat percentage and improvement in cardiorespiratory fitness. Reinforcing these findings, a recent meta-analysis with 15 longitudinal studies demonstrated that HIIT significantly improved cardiorespiratory fitness [VO2max 1.117 (95% CI = 0.528 to 1.706, p < .001)] and reduced body weight [-0.295 (95% CI = 0.525 to -0.066, p < .05)] and body fat [-0.786 (95% CI = -1.452 to -0.120)] in children and teenagers of 6 to 18 years with obesity/overweight (Thivel et al., 2019). Additionally, an intervention of 12 weeks comparing HIIT, recreational soccer, and a control group indicated a positive effect on body composition, and an increase in lower limb strength, agility, and flexibility of overweight/obese males between 11 and 13 years of age (Cvetković et al., 2018).
Furthermore, through a cross-sectional study, researchers identified that obese children presented lower performance in flexibility than their normal weight peers (Bataweel & Ibrahim, 2020). Similarly, the present study did not observe an intervention effect on flexibility performance, probably due to the lack of a specific focus targeting this physical ability.
Regarding intervention models and strategies with a focus on overweight pediatric groups, the school environment is highlighted (Yuksel et al., 2020). Performing recreational and play activities with content that develops motor competence and keeps children active is indispensable. Thus, adherence to structured activities during school time or recess can be efficient for improving the health of children (Metos & Murtaugh, 2011). Furthermore, a cross-sectional study verified that organized physical activities are important contributors to motor skills and physical fitness in children, supporting the need for the provision of opportunities to practice daily organized physical activities, with school physical education programs representing an ideal environment for this objective (Hardy et al., 2014).
However, when investigating physical education classes and their possibilities, studies pointed out that the number of weekly classes and the intensity reached are not sufficient and are not efficient compared to extra activities to improve fitness parameters (Gallotta et al., 2017; Walker et al., 2018), remaining below the recommendations proposed by Childhood physical activity guidelines (Leitão et al., 2000). In this context, Thivel et al. (2011) proposed two extra classes per week of 60 minutes with playful activities to improve coordination, flexibility, strength, speed, and endurance, with positive results on obesity prevention through improvement in the aerobic and anaerobic fitness of children of 6 to 10 years (Thivel et al., 2011). Moreover, proposals to add 15 minute periods of functional and calisthenic movements before class (Faigenbaum et al., 2015), participation in 2 hours per week in supervised group sports (Queiroz et al., 2014), additions of four vigorous physical activities of 60 minutes a week (Dallolio et al., 2016), and more active and intense standardized warm ups during physical education classes (Thomas et al., 2020) were shown to be efficient interventions with obese children.
In the present study, improvements in abdominal muscle fitness and cardiorespiratory condition were observed after a recreational intervention in addition to physical education classes with overweight children during 12 weeks, such as observed in another Brazilian study with sports activities twice a week, for children between 8 and 11 years old. Corroborating our findings, Ordóñez et al. (2019) in schools in Madrid, observed a significant improvement in cardiorespiratory capacity and motor coordination in children aged 11 to 12 years who participated in activities additional to Physical Education classes. Gonçalves et al. (2019) reported a reduction in relative fat and BMI and improvement in all physical fitness scores, including strength, endurance, and flexibility (Gonçalves et al., 2019). Previously, other studies demonstrated the efficiency of extracurricular interventions on weight and waist perimeter reductions in children, as well as improvements in physical fitness (Jansen et al., 2011). Furthermore, activities applied in the classroom significantly increased habitual physical activity levels of children (Reznik et al., 2015), and decreased BMI percentiles (Sharma et al., 2019).
Increasing physical fitness scores have special importance due to the reverse relation with overweight. Thus, a longitudinal study of 20 years following 1792 individuals between 7 and 15 years of age stated that low cardiorespiratory fitness is related to higher waist circumference (Schmidt et al., 2016). Similarly, Ruedl et al. (2018) observed that overweight and obese children have lower levels of physical fitness in comparison to normal weight children. Moreover, children presenting an improvement in health-related physical fitness and motor competence during childhood are less likely to develop overweight or obesity conditions (Rodrigues et al., 2016). Corroborating these assumptions, a prospective study reassessed the cardiorespiratory fitness of 647 individuals, stating that the lower the aerobic fitness, the higher the chances of becoming obese [OR 3.0 (95% CI 1.6-5.6)], and concerning elevated obesity, the likelihood of a reduction in physical fitness is higher between childhood and adulthood [OR 4.5 (95% CI 2.6-7.7)] (Dwyer et al., 2009). This highlights the importance of an active lifestyle that continues with child growth, providing continuity of physical activity during lifespan (Telama et al., 2014).
Regarding motor competence aspects, the scenario is very similar, since being overweight causes a negative impact on children’s motor competence (Prskalo et al., 2015). Lima et al. (2019) reported an inverse relation of body fat and motor coordination, where children aged between 6 and 13 years with better motor coordination presented less body fat (Lima et al., 2019). Similarly, Augustijn et al. (2018) performed a multiprofessional intervention with obese children between 7 and 11 years of age. The results demonstrated that obese children presented lower levels of motor competence, manual dexterity, and static/dynamic balance, and presented more difficulty planning and controlling movements compared to healthy weight peers.. In another study, the association between motor competence and body composition was investigated in a group of 70 children of 6 to 10 years of age. The results showed that the motor proficiency of children was negatively associated with the amount of body fat. In addition, the study evidenced that normal weight children presented better motor competence in gross motor skills than overweight children (Marmeleira et al., 2017).
Notwithstanding, Zanella et al. (2016) discovered that a motor intervention program of 32 sessions significantly improved the motor domains of overweight and obese children between 6 and 8 years of age.
In the present study, despite the small sample size and the absence of a control group, the results demonstrated important responses to the 12-week recreational activities protocol in overweight children. Our findings indicate a significant reduction in relative and abdominal fat with improvement in the ability to move and control objects, reflecting positively on the general motor quotient. This particular outcome was shown by Barnett et al. (2009) to have great relevance, since proficiency in fundamental motor skills, mainly object control, subsequently predicted the time spent on moderate and vigorous physical activity in adolescence.
Lastly, from the authors’ perspective, there are two strong findings. First, the efficiency of the intervention protocol in school to reduce central and total adiposity, and secondly, the positive effect on motor competence, and muscle and cardiorespiratory fitness levels, that together increase the chances of the incorporation of healthy habits and physical activities now and in future life.
Conclusions
The present study found a positive effect of a school intervention protocol with recreational motor activity on body weight control, motor competence, and cardiorespiratory and muscular physical fitness. The findings suggest that future investigations should confirm the impact of school interventions in the context of physical and motor activities on body weight control during childhood.
Author note
The authors declare that this is an original article; Not published elsewhere in its whole or partly; It’s not in evaluation process in any other publication; We are responsible for the final version of this article; If accepted for publication, all authors’s copyright are transferred to the Institut Nacional d’Educació Física de Catalunya (INEFC), assuming all exclusive rights to edit, publish or reproduce it in any format; And that we have no conflict of interests.
References
[1] Aiello, A. M., Marques de Mello, L., Souza Nunes, M., Soares da Silva, A., & Nunes, A. (2015). Prevalence of obesity in children and adolescents in Brazil: a meta-analysis of cross-sectional studies. Current Pediatric Reviews, 11(1), 36-42. doi.org/10.2174/1573396311666150501003250
[2] Augustijn, M. J., D’Hondt, E., Van Acker, L., De Guchtenaere, A., Lenoir, M., Caeyenberghs, K., & Deconinck, F. J. (2018). Role of motor competence and executive functioning in weight loss: a study in children with obesity. Journal of Developmental & Behavioral Pediatrics, 39(8), 642-651. doi.org/10.1097/dbp.0000000000000589
[3] Bacchini, D., Licenziati, M. R., Garrasi, A., Corciulo, N., Driul, D., Tanas, R., & Maltoni, G. (2015). Bullying and victimization in overweight and obese outpatient children and adolescents: an Italian multicentric study. PLoS One, 10(11), e0142715. doi.org/10.1371/journal.pone.0142715
[4] Barnett, L. M., Van Beurden, E., Morgan, P. J., Brooks, L. O., & Beard, J. R. (2009). Childhood motor skill proficiency as a predictor of adolescent physical activity. Journal of Adolescent Health, 44(3), 252-259. doi.org/10.1016/j.jadohealth.2008.07.004
[5] Bataweel, E. A., & Ibrahim, A. I. (2020). Balance and musculoskeletal flexibility in children with obesity: a cross-sectional study. Annals of Saudi Medicine, 40(2), 120-125. doi.org/10.5144/0256-4947.2020.120
[6] Bravo, A., Foley, B. C., Innes-Hughes, C., O’Hara, B. J., & Rissel, C. (2020). The equitable reach of a universal, multisector childhood obesity prevention program (Live Life Well@ School) in Australian primary schools. Public Health Research & Practice, 30(1). doi.org/10.17061/phrp3012003
[7] Brusseau, T. A., Hannon, J. C., Fu, Y., Fang, Y., Nam, K., Goodrum, S., & Burns, R. D. (2018). Trends in physical activity, health-related fitness, and gross motor skills in children during a two-year comprehensive school physical activity program. Journal of Science and Medicine in Sport, 21(8), 828-832. doi.org/10.1016/j.jsams.2017.12.015
[8] Carlson, J. A., Engelberg, J. K., Cain, K. L., Conway, T. L., Mignano, A. M., Bonilla, E. A., & Sallis, J. F. (2015). Implementing classroom physical activity breaks: Associations with student physical activity and classroom behavior. Preventive Medicine, 81, 67-72. doi.org/10.1016/j.ypmed.2015.08.006
[9] Cattuzzo, M. T., dos Santos Henrique, R., Ré, A. H. N., de Oliveira, I. S., Melo, B. M., de Sousa Moura, M., & Stodden, D. (2016). Motor competence and health related physical fitness in youth: A systematic review. Journal of Science and Medicine in Sport, 19(2), 123-129. doi.org/10.1016/j.jsams.2014.12.004
[10] Cvetković, N., Stojanović, E., Stojiljković, N., Nikolić, D., Scanlan, A. T., & Milanović, Z. (2018). Exercise training in overweight and obese children: Recreational football and high-intensity interval training provide similar benefits to physical fitness. Scandinavian Journal of Medicine & Science in Sports, 28, 18-32. doi.org/10.1111/sms.13241
[11] Da Costa, B. G., da Silva, K. S., George, A. M., & de Assis, M. A. A. (2017). Sedentary behavior during school-time: Sociodemographic, weight status, physical education class, and school performance correlates in Brazilian schoolchildren. Journal of Science and Medicine in Sport, 20(1), 70-74. doi.org/10.1016/j.jsams.2016.06.004
[12] Dallolio, L., Ceciliani, A., Sanna, T., Garulli, A., & Leoni, E. (2016). Proposal for an enhanced physical education program in the primary school: evaluation of feasibility and effectiveness in improving physical skills and fitness. Journal of Physical Activity and Health, 13(10), 1025-1034. doi.org/10.1123/jpah.2015-0694
[13] Delgado-Floody, P., Espinoza-Silva, M., García-Pinillos, F., & Latorre-Román, P. (2018). Effects of 28 weeks of high-intensity interval training during physical education classes on cardiometabolic risk factors in Chilean schoolchildren: a pilot trial. European Journal of Pediatrics, 177(7), 1019-1027. doi.org/10.1007/s00431-018-3149-3
[14] Dwyer, T., Magnussen, C. G., Schmidt, M. D., Ukoumunne, O. C., Ponsonby, A. L., Raitakari, O. T., & Venn, A. (2009). Decline in physical fitness from childhood to adulthood associated with increased obesity and insulin resistance in adults. Diabetes Care, 32(4), 683-687. doi.org/10.2337/dc08-1638
[15] Engel, A. C., Broderick, C. R., van Doorn, N., Hardy, L. L., & Parmenter, B. J. (2018). Exploring the relationship between fundamental motor skill interventions and physical activity levels in children: A systematic review and meta-analysis. Sports Medicine, 48(8), 1845-1857. doi.org/10.1007/s40279-018-0923-3
[16] Errisuriz, V. L., Golaszewski, N. M., Born, K., & Bartholomew, J. B. (2018). Systematic review of Physical Education-based physical activity interventions among elementary school children. The Journal of Primary Prevention, 39(3), 303-327. doi.org/10.1007/s10935-018-0507-x
[17] Faigenbaum, A. D., Bush, J. A., McLoone, R. P., Kreckel, M. C., Farrell, A., Ratamess, N. A., & Kang, J. (2015). Benefits of strength and skill-based training during primary school physical education. The Journal of Strength & Conditioning Research, 29(5), 1255-1262. doi.org/10.1519/jsc.0000000000000812
[18] Gallotta, M. C., Emerenziani, G. P., Iazzoni, S., Iasevoli, L., Guidetti, L., & Baldari, C. (2017). Effects of different physical education programmes on children’s skill-and health-related outcomes: a pilot randomised controlled trial. Journal of Sports Sciences, 35(15), 1547-1555. doi.org/10.1080/02640414.2016.1225969
[19] García-Marín, P., & Fernández-López, N. (2020). Motor Skills Competence in Preschool Education. Apunts Educación Física y Deportes, 141, 21-32. doi.org/10.5672/apunts.2014-0983.es.(2020/3).141.03
[20] Gaya, A., & Gaya, A. R. (2016). Projeto esporte Brasil: manual de testes e avaliação. Porto Alegre: UFRGS, 1-26.
[21] Gonçalves, M. J. R., Santos, C. R., & Silva, C. C. (2019). The impact of systematized physical activity on parameters of health-related physical fitness in schoolchildren aged 8 to 11 years. Revista Brasileira de Atividade Física & Saúde, 24, 1-7. doi.org/10.12820/rbafs.24e0072
[22] Greulich, W. W., & Pyle, S. I. (1959). Radiographic Atlas of Skeletal Development of the Hand and Wrist. Stanford university press.
[23] Gu, X., Chang, M., & Solmon, M. A. (2016). Physical activity, physical fitness, and health-related quality of life in school-aged children. Journal of Teaching in Physical Education, 35(2), 117-126. doi.org/10.1123/jtpe.2015-0110
[24] Hardy, L. L., O’Hara, B. J., Rogers, K., St George, A., & Bauman, A. (2014). Contribution of organized and nonorganized activity to children’s motor skills and fitness. Journal of School Health, 84(11), 690-696. doi.org/10.1111/josh.12202
[25] Henrique, R. S., Ré, A. H., Stodden, D. F., Fransen, J., Campos, C. M., Queiroz, D. R., & Cattuzzo, M. T. (2016). Association between sports participation, motor competence and weight status: A longitudinal study. Journal of Science and Medicine in Sport,19(10), 825-829. doi.org/10.1016/j.jsams.2015.12.512
[26] Henrique, R. S., Stodden, D. F., Fransen, J., Feitoza, A. H., Ré, A. H., Martins, C. M., & Cattuzzo, M. T. (2020). Is motor competence associated with the risk of central obesity in preschoolers? American Journal of Human Biology, 32(3), e23364. doi.org/10.1002/ajhb.23364
[27] Jansen, W., Borsboom, G., Meima, A., Zwanenburg, V. J. V., Mackenbach, J. P., Raat, H., & Brug, J. (2011). Effectiveness of a primary school-based intervention to reduce overweight. International Journal of Pediatric Obesity, 6(sup3), e70-77. doi.org/10.3109/17477166.2011.575151
[28] Kari, J. T., Tammelin, T. H., Viinikainen, J., Hutri-Kähönen, N., Raitakari, O. T., & Pehkonen, J. (2016). Childhood physical activity and adulthood earnings. Medicine and Science in Sports and Exercise, 48(7). doi.org/10.1249/mss.0000000000000895
[29] Kuczmarski, R. J. (2002). 2000 CDC Growth Charts for the United States: methods and development (No. 246). Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
[30] Leitão, M. B., Lazzoli, J. K., Oliveira, M. A. B. D., Nóbrega, A. C. L. D., Silveira, G. G. D., Carvalho, T. D., ... & Drummond, F. A. (2000). Posicionamento oficial da Sociedade Brasileira de Medicina do Esporte: atividade física e saúde na mulher. Revista Brasileira de Medicina do Esporte, 6(6), 215-220. doi.org/10.1590/S1517-86921999000600002
[31] Lima, R. A., Bugge, A., Ersbøll, A. K., Stodden, D. F., & Andersen, L. B. (2019). The longitudinal relationship between motor competence and measures of fatness and fitness from childhood into adolescence. Jornal de Pediatria, 95(4), 482-488. doi.org/10.1016/j.jpedp.2018.06.007
[32] Mahon, A. D., Marjerrison, A. D., Lee, J. D., Woodruff, M. E., & Hanna, L. E. (2010). Evaluating the prediction of maximal heart rate in children and adolescents. Research Quarterly for Exercise and Sport, 81(4), 466-471. doi.org/10.1080/02701367.2010.10599707
[33] Marmeleira, J., Veiga, G., Cansado, H., & Raimundo, A. (2017). Relationship between motor proficiency and body composition in 6-to 10-year-old children. Journal of Paediatrics and Child Health, 53(4), 348-353. doi.org/10.1111/jpc.13446
[34] Metos, J., & Murtaugh, M. (2011). Words or reality: Are school district wellness policies implemented? A systematic review of the literature. Childhood Obesity (Formerly Obesity and Weight Management), 7(2), 90-100. doi.org/10.1089/chi.2011.07.02.0514.metos
[35] Mosca, L. N., Goldberg, T. B. L., da Silva, V. N., Kurokawa, C. S., Rizzo, A. C. B., da Silva, C. C., ... & Corrente, J. E. (2017). The impact of excess body fat on bone remodeling in adolescents. Osteoporosis International, 28(3), 1053-1062. doi.org/10.1007/s00198-016-3838-6
[36] Nemet, D. (2018). Childhood Obesity, Physical Activity, and Exercise–The Year That Was 2017: Normal-Weight Obese–Are We Missing a Population in Need? Pediatric Exercise Science, 30(1), 52-53. doi.org/10.1123/pes.2018-0005
[37] Ordóñez, A. F., Polo, B., Lorenzo, A., & Shaoliang, Z. (2019). Effects of a School Physical Activity Intervention in Pre-adolescents. Apunts. Educación Física y Deportes, 136, 49-61. dx.doi.org/10.5672/apunts.2014-0983.es.(2019/2).136.04
[38] Prskalo, I., Badrić, M., & Kunješić, M. (2015). The percentage of body fat in children and the level of their motor skills. Collegium Antropologicum, 39(Supplement 1), 21-28. doi.org/10.1159/000477406
[39] Queiroz, D. D. R., Ré, A. H. N., Henrique, R. D. S., Moura, M. D. S., & Cattuzzo, M. T. (2014). Participation in sports practice and motor competence in preschoolers. Motriz: Revista de Educação Física, 20(1),26-32. doi.org/10.1590/S1980-65742014000100004
[40] Ré, A. H. N., Tudela, M. C., Monteiro, C. B. D. M., Antonio, B. D. A., Silva, M. M. D. L. M., Campos, C. M. C., & Cattuzzo, M. T. (2018). Motor competence of schoolchildren from public education in São Paulo city, Brazil. Journal of Physical Education, 29. doi.org/10.4025/jphyseduc.v29i1.2955
[41] Reulbach, U., Ladewig, E. L., Nixon, E., O’Moore, M., Williams, J., & O’Dowd, T. (2013). Weight, body image and bullying in 9-year-old children. Journal of Paediatrics and Child Health, 49(4), E288-E293. doi.org/10.1111/jpc.12159
[42] Reznik, M., Wylie-Rosett, J., Kim, M., & Ozuah, P. O. (2015). A classroombased physical activity intervention for urban kindergarten and firstgrade students: a feasibility study. Childhood Obesity, 11(3), 314-324. doi.org/10.1089/chi.2014.0090
[43] Rodrigues, L. P., Stodden, D. F., & Lopes, V. P. (2016). Developmental pathways of change in fitness and motor competence are related to overweight and obesity status at the end of primary school. Journal of Science and Medicine in Sport, 19(1), 87-92. doi.org/10.1016/j.jsams.2015.01.002
[44] Ruedl, G., Franz, D., Frühauf, A., Kopp, M., Niedermeier, M., Drenowatz, C., & Greier, K. (2018). Development of physical fitness in Austrian primary school children. Wiener Klinische Wochenschrift, 30(9-10), 321-327. doi.org/10.1007/s00508-018-1336-x
[45] Schmidt, M. D., Magnussen, C. G., Rees, E., Dwyer, T., & Venn, A. J. (2016). Childhood fitness reduces the long-term cardiometabolic risks associated with childhood obesity. International Journal of Obesity, 40(7), 1134-1140. doi.org/10.1038/ijo.2016.61
[46] Sentalin, P. B. R., de Oliveira Pinheiro, A., de Oliveira, R. R., Zângaro, R. A., Campos, L. A., & Baltatu, O. C. (2019). Obesity and metabolic syndrome in children in Brazil: the challenge of lifestyle change. Medicine, 98(19). doi.org/10.1097/md.0000000000015666
[47] Sharma, S. V., Vandewater, E., Chuang, R. J., Byrd-Williams, C., Kelder, S., Butte, N., & Hoelscher, D. M. (2019). Impact of the coordinated approach to child health early childhood program for obesity prevention among preschool children: The Texas childhood obesity research demonstration study. Childhood Obesity, 15(1), 1-13. doi.org/10.1089/chi.2018.0010
[48] Slaughter, M. H., Lohman, T. G., Boileau, R., Horswill, C. A., Stillman, R. J., Van Loan, M. D., & Bemben, D. A. (1988). Skinfold equations for estimation of body fatness in children and youth. Human biology, 709-723.
[49] Stodden, D. F., Goodway, J. D., Langendorfer, S. J., Roberton, M. A., Rudisill, M. E., Garcia, C., & Garcia, L. E. (2008). A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship, Quest, 60:2, 290-306. doi.org/10.1080/00336297.2008.10483582
[50] Telama, R., Yang, X., Leskinen, E., Kankaanpaa, A., Hirvensalo, M., Tammelin, T., & Raitakari, O. T. (2014). Tracking of physical activity from early childhood through youth into adulthood. Medicine & Science in Sports & Exercise, 46(5), 955-962. doi.org/10.1249/mss.0000000000000181
[51] Thivel, D., Isacco, L., Lazaar, N., Aucouturier, J., Ratel, S., Doré, E., ... & Duché, P. (2011). Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. European Journal of Pediatrics, 170(11), 1435-1443. doi.org/10.1007/s00431-011-1466-x
[52] Thivel, D., Masurier, J., Baquet, G., Timmons, B. W., Pereira, B., Berthoin, S., & Aucouturier, J. (2019). High-intensity interval training in overweight and obese children and adolescents: systematic review and meta-analysis. The Journal of Sports Medicine and Physical Fitness, 59(2), 310-324. doi.org/10.23736/s0022-4707.18.08075-1
[53] Thomas, E., Bianco, A., Tabacchi, G., Marques da Silva, C., Loureiro, N., Basile, M., & Gómez-López, M. (2020). Effects of a physical activity intervention on physical fitness of schoolchildren: the enriched sport activity program. International Journal of Environmental Research and Public Health, 17(5), 1723. doi.org/10.3390/ijerph17051723
[54] Ulrich, D. (2000). The test of gross motor development. Austin, TX: Prod-Ed. Valentini, N. C. (2012). Validity and reliability of the TGMD-2 for Brazilian children. Journal of Motor Behavior, 44(4), 275-280. doi.org/10.1080/00222895.2012.700967
[55] Valentini, N. C., Nobre, G. C., de Souza, M. S., & Duncan, M. J. (2020). Are BMI, Self-Perceptions, Motor Competence, Engagement, and Fitness Related to Physical Activity in Physical Education Lessons? Journal of Physical Activity and Health, 17(5), 493-500. doi.org/10.1123/jpah.2019-0532
[56] Vandorpe, B., Vandendriessche, J., Vaeyens, R., Pion, J., Matthys, S., Lefevre, J., & Lenoir, M. (2012). Relationship between sports participation and the level of motor coordination in childhood: A longitudinal approach. Journal of Science and Medicine in Sport, 15(3), 220-225. doi.org/10.1016/j.jsams.2011.09.006
[57] Walker, G., Stracciolini, A., Faigenbaum, A. D., & Myer, G. D. (2018). Physical Inactivity in Youth: Can Exercise Deficit Disorder Alter the Way We View Preventative Care? ACSM’s Health & Fitness Journal, 22(2), 42-46. doi.org/10.1249/FIT.0000000000000370
[58] Yuksel, H. S., Şahin, F. N., Maksimovic, N., Drid, P., & Bianco, A. (2020). School-Based Intervention Programs for Preventing Obesity and Promoting Physical Activity and Fitness: A Systematic Review. International Journal of Environmental Research and Public Health, 17(1), 347. doi.org/10.3390/ijerph17010347
[59] Zanella, L. W., Sousa, M. S. D., Bandeira, P. F. R., Nobre, G. C., & Valentini, N. C. (2016). Crianças com sobrepeso e obesidade: intervenção motora e suas influências no comportamento motor. Motricidade, 12, S1- 42-53.
ISSN: 2014-0983
Received: January 11, 2021
Accepted: June 21, 2021
Published: January 01, 2022
Editor: © Generalitat de Catalunya Departament de la Presidència Institut Nacional d’Educació Física de Catalunya (INEFC)
© Copyright Generalitat de Catalunya (INEFC). This article is available from url https://www.revista-apunts.com/. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/deed.en


