Blood Pressure Responses in Hypertensive Women to Water Aerobics
Bruna P. Almada
*Corresponding author: Cristine Lima Alberton tinialberton@yahoo.com.br
Cite this article
Kruel, L.F.M., Bgeginski, R., Kanitz, A.C., Pinto, S.S., Almada, B.P., Finatto, P. & Alberton C.L. (2021). Blood Pressure Responses in Hypertensive Women to Water Aerobics. Apunts. Educación Física y Deportes, 144, 25-32. https://doi.org/10.5672/apunts.2014-0983.es.(2021/2).144.04
Abstract
Background: To evaluate acute blood pressure (BP) responses of hypertensive women during and 20 min after continuous (CON) and interval (INT) water aerobics sessions.
Methods: Nine treated hypertensive women (61.22 ± 2.91 years, body mass index 28.70 ± 4.45 kg.m-2) performed two randomized water-based exercise sessions (32 min): CON (13-14 Borg Scale) and INT protocol (2 min at 17 Borg Scale with 2 min of active recovery at index 9). BP was measured 20 min before, during and after exercise. Repeated measures two-way ANOVA with Bonferroni was used (α = .05).
Results: BP responses did not differ between the protocols (p > .05). For diastolic BP, halftime and endpoint exercise were significantly lower than all four recovery points measured (p < .001). A trend in p value was observed for systolic BP (p = .051), however, no differences between the time-points were found. No significant differences were observed for time-points in mean BP (p > .05).
Conclusion: Hypertensive women do not present significant difference for the BP values between CON and INT protocols, and no post-exercise hypotension was observed within 20 minutes of recovery. Thus, both protocols appear to be safely performed by treated hypertensive women.
Introduction
Hypertension has high medical and socioeconomic costs, mainly due to its complications, such as cerebrovascular and coronary artery disease, heart failure, chronic renal failure, and extremity vascular disease (Whelton et al., 2018). Data from 2013-2014 show that 33.5 % of adults aged 20 and over were diagnosed with hypertension in United States, resulting in more than 360,000 American deaths included high blood pressure (BP) as a primary or contributing cause (Mozaffarian et al., 2015), which means almost 1,000 deaths each day.
In the general population, exercise protocols with a richer variety of motor skills are more likely to favor participant interaction and engagement, and improve cardiac responses (Castañer et al., 2017). In addition, regular aerobic exercise reduces BP along training programs and the hypotensive effect is greater the higher the initial BP (Pescatello et al., 2004). Decreases in catecholamines and total peripheral resistance, improved insulin sensitivity, and alterations in vasodilators and vasoconstrictors are some of the postulated explanations for the antihypertensive effects of exercise. Emerging data suggest genetic links to the BP reductions associated with acute and chronic exercise (Pescatello et al., 2004). For this reason, increased physical activity with a structured exercise program has been widely indicated as an efficient non-pharmacological alternative for the hypertensive population (Whelton et al., 2018).
Physical exercise in the aquatic environment can be highlighted as a suitable modality for this population. It is practiced specially by women, whose responses to exercise deserve attention in literature, since they present physiological, morphological, and psychological differences in comparison to men (Gómez-Jiménez & López de Subijana-Hernández, 2016; González Robles et al., 2017; Granda Vera et al. 2018). Moreover, immersion may induce a reduction in BP in normotensive individuals at rest (Srámek et al., 2000). This reduction occurs due to an immediate redistribution of blood from the periphery to the central region of the body, causing an increase in cardiac output, with a consequent increase in renal blood flow, and which, concomitantly with a decrease in plasma renin activation and an increase in the peptide concentration atrial natriuretic, cause reduction of BP values (Rim et al., 1997). Moreover, in the last few years some studies have observed the chronic effect of aquatic training on BP responses (Guimarães et al., 2014). A 36-week water-based exercises program was able to promote a reduction of 36 mmHg in systolic BP (SBP) and 12 mmHg in diastolic BP (DBP) in resistant and medicated hypertensive patients (Guimarães et al., 2014).
The chronic reduction in BP with regular exercise seems to be partially explained by acute BP decreases after a session of exercise. Studies have demonstrated aerobic physical exercises performed on land present a significant acute reduction in post-exercise BP responses (MacDonald et al., 1999), a phenomenon known as post-exercise hypotension (PEH). In addition, different protocols of water-based exercises have been investigated in order to verify the presence of PEH in normotensive and hypertensive individuals (Bocalini et al., 2017; Cunha et al., 2017; Cunha et al., 2018; Pinto et al., 2017; Pontes-Júnior et al., 2008; Rodriguez et al., 2011; Sosner et al., 2016; Terblanche and Millen, 2012). Regarding acute PEH in aquatic exercise sessions, Rodriguez et al. (2011) and Pinto et al. (2017) evaluated the BP 60 min after water-walking and water-based concurrent training in normotensive participants, respectively, while Cunha et al. (2012, 2017), Pontes-Junior et al. (2008), and Bocalini et al. (2017) from 10 to 90 min after water-based aerobic sessions in individuals with prehypertension and hypertension. Regarding 24h-PEH, Cunha et al. (2018) evaluated it after water-based exercises in normotensive women over 65 years, and Terblanche and Millen (2012) and Sosner et al. (2016) in individuals with prehypertension and hypertension. From these studies, Sosner et al. (2016) was the only one who employed an interval water-based protocol; however, their purpose was to compare PEH from different environments (dry land versus water).
In addition to the environment in which exercise is performed, another factor that may influence the PEH phenomenon is the intensity of the training session in healthy (Angadi et al., 2015) and hypertensive (Ciolac et al., 2009) individuals. Ciolac et al. (2009) analyzed the BP responses after a 40 min continuous (60 % reserve HR) and interval (1 min 80 % and 2 min 50 % reserve HR) cycling protocol performed on land. The authors observed a significant reduction in PEH 24h-systolic and nighttime SBP and a trend to reduce nighttime DBP in the interval protocol. However, the effects of different intensities during water-based exercise protocols (i.e., continuous moderate intensity versus interval high intensity) on PEH in individual with hypertension remain unclear in the literature. The optimal training intensity needs to be better defined to optimize the BP lowering capacities of exercise.
Therefore, the purpose of the present study was to evaluate acute BP responses of treated hypertensive women during and 20 min after continuous and interval water-based exercise protocols. We hypothesized that higher intensity exercise could induce greater reduction in BP responses, evidencing a significant acute PEH.
Methods
Participants
The sample was composed by nine women, volunteers, diagnosed with hypertension by a physician during a clinical evaluation following the cut-off points: SBP ≥ 140 mmHg and DBP ≥ 90 mmHg. Eligibility criteria were: 1) diagnose of hypertension for at least 6 months; 2) be physically active for at least 6 months; 3) treated with medication but not β-blockers; 4) not smoke; 5) no physical limitations; 6) should be familiarized to aquatic exercises.
Upon starting the research, all participants signed an informed consent form. The study was approved by the Research Ethics Committee of the Federal University of Rio Grande do Sul, Brazil (2008168).
Experimental procedures
The present is a pilot study, with a crossover trial design. Each woman participated in three sessions, with a minimum interval of 48h between sessions. The first session was designed to familiarize and characterize the participants, and the other two sessions to the experimental protocols, performed at random order. The experimental protocols corresponded to a continuous (CON) and interval (INT) water-based exercise sessions. Heart rate (HR) and BP were measured 20 min before, during, and 20 min after exercise, with one measure every 5 min. Figure 1 shows the schematic flowchart of the data collection protocol.
Participant characteristics
Participants were 61.22 ± 2.91 years, 72.00 ± 16.40 kg, 157.72 ± 7.55 cm, body mass index 28.70 ± 4.45 kg.m-2, considered as slightly overweighted. The hypertension was pharmacologically controlled with calcium channel blockers: n = 1; angiotensin converting enzyme inhibitors: n = 5; diuretic: n = 3.

Characterization and familiarization
In the initial session, body mass (kg) and height (m) were measured using a scale and a stadiometer (Filizola, São Paulo, Brazil). In this session, the participants were familiarized with the BP device, the 6-20 Borg Scale (Borg, 1990), and with the exercises. Participants were instructed to observe the degree of tension and fatigue in their muscles, shortness of breath and chest pain. The 15-point scale was explained considering it incorporates nine verbal descriptors ranging from “no exertion at all” (RPE 6) to “maximal exertion” (RPE 20). A rating of 6 corresponds to the level of exertion experienced during a quiet seated rest, whilst a rating of 19 approximates maximal or near-maximal physical exertion (Borg, 1990). The scale (60 × 90 cm banner) was placed out of the pool in front of the participant during the familiarization e protocol sessions. All the details of execution and amplitude of the movements were explained and then, the women performed the exercises at a comfortable pace. The familiarization session was finalized with the drawing of the execution order of the exercise protocols (CON or INT).
The HR (HR monitor model F6TM; Polar, Kempele, Finland), SBP and DBP (BP monitor ABPM-04 recorder with mean arterial pressure optical interface, Meditech, Budapest, Hungary, respectively) were monitored before, halftime exercise and after the protocols. The mean BP (MBP) was calculated using the formula MBP = DBP + [0.333 * (SBP-DBP)].
Interventions and outcome measurements
Regardless of the protocol, the participants always started remaining at rest out of the water, in the seated position for 20 min, with their feet and arms supported, and the chair positioned at the edge of the pool near the stairs. The HR and BP measurements were performed every 5 min during this period. For the analysis of the resting situation, the values of the 10th minute of the seated rest were used.
Water-based exercise protocols were performed during 32 min with the intensity prescribed by the rating of perceived exertion (RPE) based on 6-20 Borg scale (Borg, 1990). In the CON protocol, the intensity was controlled by RPE between 13 and 14 (somewhat hard). In the INT protocol, eight 2 min bouts at RPE 17 (very hard) were interspersed by 2 min of active recovery at RPE 9 (very light). Both CON and INT protocols were composed by two blocks of four exercises, each one performed for 4 min, totaling 32 min of exercise. The following sequence of water-based exercises were used: stationary running with simultaneous elbow flexion and extension, cross country skiing with simultaneous shoulders flexion and extension, jumping jacks with simultaneous shoulders abduction and adduction, and frontal kick up to 45º with simultaneous arms pushing the water forward. This protocol model was previously used in the study by Kruel et al. (2009) whose objective was to analyze the cardiorespiratory responses between protocols. The experimental sessions were always applied by the same instructor to a maximum of two participants per period, without background music.
The HR and BP evaluations during the protocols were performed at 16 min (halftime) and immediately at the end of session (endpoint). Protocols were performed in a pool with a depth variation of 0.95 to 1.30 m, allowing each of the participants to be immersed in the xiphoid process depth. The water temperature was maintained between 31° and 32° C.
Similar to the initial phase, after the end of the exercise protocol the participants rested out of the water, in the seated position for 20 min, with their feet and arms supported, and the chair positioned at the edge of the pool near the stairs. The HR and BP measurements were performed every 5 min during this period. For the analysis of the post-exercise seated situation, the values of the 10th minute of the seated rest were used.
Statistical analysis
Descriptive statistics (mean ± standard deviation) and Shapiro-Wilk’s normality test were used.
Repeated measures two-way ANOVA (protocol and time-points) with Bonferroni post-hoc was used to compare the outcomes between the tested situations. When the interaction was significant, the F test was performed for each main effect. The effect size for each main effect was calculated by ηp2. The significance level was set to α = .05. All statistical tests were performed in the Statistical Package for Social Sciences software (version 20.0 for Windows; SPSS Inc., Chicago, IL, USA).

Results
Blood pressure and heart rate responses at rest
The pre-exercise rest situation for day 1 and day 2 were similar. The mean values of SBP, DBP, MBP, and HR at pre-exercise rest were 121.88 ± 12.87 mmHg, 74.66 ± 9.95 mmHg, 90.40 ± 8.97 mmHg, and 81.41 ± 16.92 bpm for the interval session, respectively, and 121.11 ± 14.34 mmHg, 72.55 ± 8.54 mmHg, 88.74 ± 9.57 mmHg, and 83.23 ± 18.86 bpm for the CONT, respectively.
Blood pressure and heart rate responses during exercise
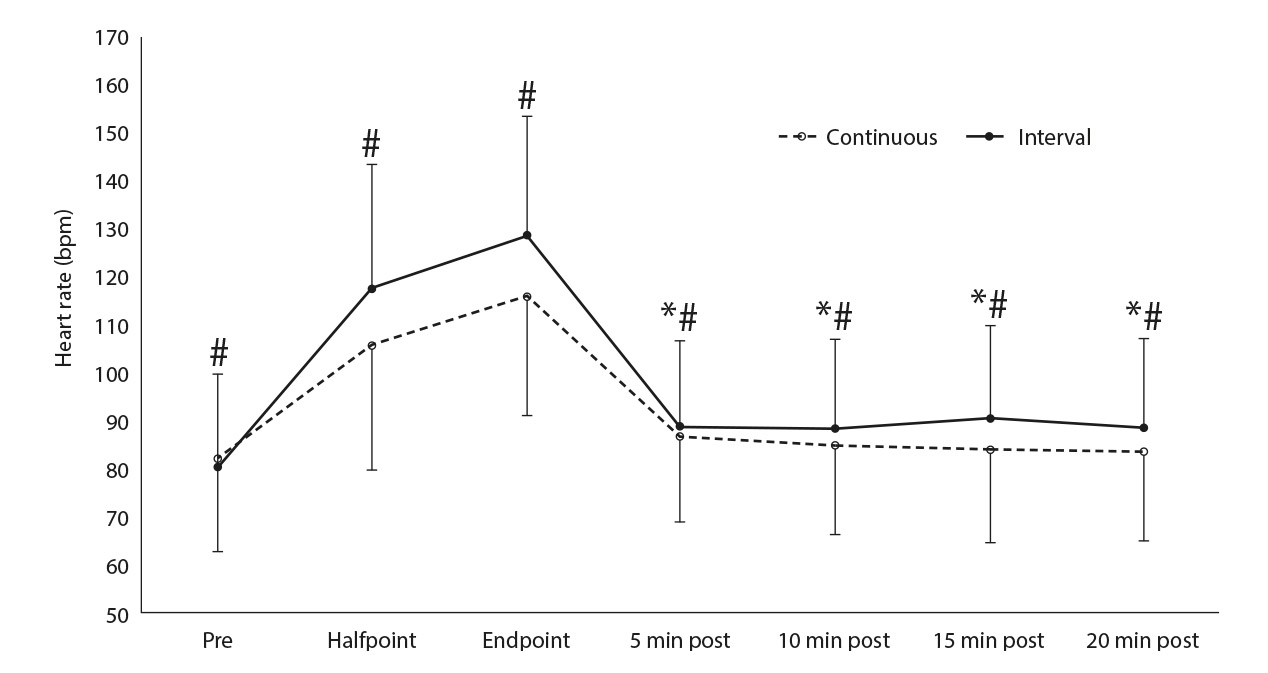
Regarding the protocols, the HR response was significant higher for INT compared to CON (halftime: 118.19 ± 26.32 bpm vs 106.51 ± 25.57 bpm, endpoint: 130.14 ± 28.49 bpm vs 116.29 ± 23.82 bpm, respectively; p = .021; ηp2 =.508; Figure 2). Blood pressure responses did not differ between the protocols during exercise (i.e., halftime and endpoint) (p > .05; Figure 3).
Blood pressure and heart rate responses post-exercise
The analyses of water-based exercises at rest (min 10), exercise (halftime and endpoint) and during recovery (5, 10, 15, 20 min) are presented in Figure 2 and 3.
The main effect time-point presented a significant difference for DBP (p < .001; ηp2 = .699) and HR (p < .001; ηp2 = 0.720). For DBP, both exercise measurements (halftime and endpoint) were significantly lower than all four recovery points measured. For HR, the endpoint exercise measurement was significantly higher than pre-exercise as well as all four recovery points measured. Regarding SBP, a trend in p value was observed (p = .051; ηp2 = .347), however, no differences between the time-points were found with post-hoc analysis. Finally, no significant differences were observed for time-points in MBP (p > .05; CONT and INT: rest pre-exercise: 88.7 ± 9.6 mmHg and 90.4 ± 9.0 mmHg, exercise halftime: 85.8 ± 10.5 mmHg and 92.0 ± 14.0 mmHg, exercise endpoint: 89.9 ± 10.1 mmHg and 91.5 ± 14.6 mmHg, post5min: 96.0 ± 8.5 mmHg and 93.8 ± 9.7 mmHg, post10min: 96.9 ± 11.2 mmHg and 92.9 ± 8.9 mmHg, post15min: 94.5 ± 12.0 mmHg and 91.9 ± 9.2 mmHg, post20min: 94.8 ± 10.4 mmHg and 94.4 ± 11.0 mmHg, respectively).
Discussion
The purpose of the present study was to evaluate BP responses of treated hypertensive women in continuous and interval water-based exercise sessions. The main findings of the present study were the absence of significant difference between the protocols (continuous vs. interval) for the BP variables, regardless the higher HR values during the exercise interval session. Another important finding is that there was no post-exercise hypotension within 20 min of recovery, in contrast to our hypothesis.
The literature reports a hypotensive post-aquatic exercise response in hypertensive individuals, which was not verified in the present study. Cunha et al. (2012, 2017), Pontes-Junior et al. (2008), and Bocalini et al. (2017) evaluated the PEH from 30 to 90 min of recovery after water-based exercise sessions. Cunha et al. (2012) evaluated elderly hypertensive women 30 min after a moderate intensity (RPE ≈13) and predominantly aerobic (40 min) water-based exercise session. The SBP decreased significantly only 30 min after the exercise session (Baseline: 135.5 mmHg; 30 min: 126.9 mmHg), while DBP decreased significantly from 76.1 at rest to 74.8, 72.6, and 72.8 mmHg at minutes 10, 20 and 30, respectively. A similar protocol was applied for the same research group in a crossover clinical trial (Cunha et al., 2017) and the results showed at 10 min after exercise, SBP and DBP significantly declined 7.5 mmHg (6.2 %) and 3.8 mmHg (5.5 %), respectively, compared to a control session (no exercise for 45 min), but at 20 and 30 min after exercise, BP were similar in both exercise and no-exercise sessions. In the present study only 20 min of recovery were evaluated and no PEH effect was observed after a water-based continuous or interval exercise session.
Pontes-Junior et al. (2008) evaluate hypertensive individuals 90 min after running in water and dry land (at 50 % of VO2peak, 45 min). SBP was reduced as early as 10 min post-exercise and presented a greater reduction at 30 min after water-based exercise (142 vs. 107 mmHg). DBP was reduced as early as 5 min after water-based exercise and presented a greater reduction at 30 min (93 vs. 76 mmHg). The greater reduction of mean arterial pressure was observed at 30 min after water-based exercise (109 vs. 86 mmHg).
This disagreement with the previous studies performed in the aquatic environment may be related to the population of the present study of hypertensive women controlled with medication, since is well-known the PEH is larger the higher the initial BP value (Pescatello et al., 2004). The participants of the present study presented a mean SBP and DBP at pre-exercise of 121.50 ± 13.22 mmHg and 73.61 ± 9.06 mmHg, respectively, lower than the SBP and DBP values found in the studies of Pontes-Junior et al. (2008) (142 ± 2 mmHg and 93 ± 2%mmHg, respectively) and Cunha et al. (2012) for the control and experimental groups (SBP: 138.25 ± 12.78%mmHg and 135.46 ± 7.42 mmHg, respectively; DBP: 74.90 ± 7.31%mmHg and 76.09 ± 6.49 mmHg, respectively).
In addition, Bocalini et al. (2017) evaluated the effect of water- and land-ergometric exercise (75 % VO2max, 45 min) sessions on PEH of healthy normotensive, treated or untreated hypertensive patients. At 90 min after the exercise session, the prevalence of hypotension was significantly higher in water than in the land-based protocol. Moreover, more pronounced reductions in SBP and DBP were observed in the untreated patients compared to treated and normotensive subjects. It is interesting that the ratio of treated patients compared to those not treated with medication also interferes with initial BP values reflecting the magnitude of PEH. In the present study, because women were pharmacologically treated, the initial BP values were lower, resulting in an absence of PEH in the first 20 min post-exercise.
Furthermore, other studies evaluated 24h-post water-based exercise. Terblanche & Millen (2012) determined and compared the magnitude and duration of PEH after an acute session of concurrent exercise in water and on dry land (60 and 80 %VO2peak, RPE 12–16, 55 min) in individuals with pre-hypertension and hypertension. The PEH response for SBP lasted for 9 h after water-based exercise session. Besides comparison of BP responses of hypertensive individuals following water-based exercises (high-intensity protocol), Sosner et al. (2016) also compared moderate-intensity continuous exercise (24-min, 50 % peak power output), and high-intensity interval exercise (two sets of 10-min with bouts of 15-sec 100 % peak power output interspersed by 15-sec of passive recovery) on dry land in stationary cycle. Dry land and immersed high-intensity exercise induced a 24-h BP decrease (SBP: -3.6 and -6.8 mmHg, DBP: -2.8 mmHg and -3.0 mmHg, respectively).
Ciolac et al. (2009) also investigated the effect of intensity on PEH in middle-aged hypertensive participants, comparing 40 min of dry land cycle ergometer exercise in continuous (60 % reserve HR) and interval (2 min at 50 % reserve HR with 1 min at 80 %) protocols. The interval protocol resulted in significant reduction on PEH 24h-systolic and nighttime systolic and tended to reduce nighttime diastolic. Therefore, the present study seems to be the first to investigate the blood pressure responses of treated hypertensive women in continuous and interval water-based exercise sessions, whose results showed that exercise sessions up to 20 min there was no PEH responses.
Nonpharmacological strategies to reduce BP was analyzed in a meta-analysis of randomized controlled trials (Herrod et al., 2018). Results from this study shown that three months of exercise-based lifestyle intervention, consisting of aerobic, resistance or combined exercise training, may produce a reduction in BP of approximately 5 mmHg SBP and 3 mmHg DBP in participants with a mean age of 65 or over. These results indicated lifestyle intervention alone cannot be recommended as a sole treatment for hypertension but may serve as a useful adjunct to pharmacotherapy because it is often the first line in management in treatment guidelines (Whelton et al., 2018).
An important limitation of the present study is the absence of an immersion control session in the aquatic environment, as well as the absence of a control group with normotensive individuals, which would help in understanding the specific BP responses of the water-based exercise protocols and the effect of the medications used. Another important limitation was the post-exercise recovery time of only 20 min. However, this was the proposal of the study, to study patients with hypertension as well as to see if the PEH phenomenon would occur immediately after the protocols. Finally, our pilot study has a low sample size which may restrict a wider generalization of the findings.
Conclusions
We conclude that controlled hypertensive women achieve higher HR values in the interval aquatic exercise session and do not present significant difference for the blood pressure values between the protocols. In addition, there was no PEH within 20 minutes of recovery for both water-based sessions.
As a practical application, we suggest that the continuous and interval water-based exercise sessions tested in this study can be performed by hypertensive individuals controlled with cardiovascular safety. Further studies should be performed by testing different intensities and exercise volumes in the water environment, to clarify which protocol could potentiate the reduction of blood pressure values in controlled hypertensive individuals and, therefore, provide a good theoretical basis for a safe prescription of aerobic training for this population.
Acknowledgments
The authors are grateful to all the participants of this project, to Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
References
[1] Angadi, S. S., Bhammar, D. M., & Gaesser, G.A. (2015). Postexercise hypotension after continuous, aerobic interval, and sprint interval exercise. Journal of Strength and Conditioning Research. 29(10), 2888-2893. doi.org/10.1519/JSC.0000000000000939.
[2] Bocalini, D. S., Bergamin, M., Evangelista, A. L., Rica, R. L., Pontes, F. L. Junior, Figueira, A. Junior., ... & Dos Santos L. (2017). Post-exercise hypotension and heart rate variability response after water- and land-ergometry exercise in hypertensive patients. PLoS One. 12(6), e0180216. doi.org/10.1371/journal.pone.0180216.
[3] Borg, G. (1990). Psychophysical scaling with applications in physical work and the perception of exertion. Scandinavian Journal of Work, Environment & Health. 16 (Suppl 1), 55–58. doi.org/10.5271/sjweh.1815.
[4] Castañer, M., Puigarnau, S., Benítez, R., Zurloni, V., & Camerino, O. (2017). How to merge observational and physiological data? A case study of motor skills patterns and heart rate in exercise programs for adult women. Anales de Psicología. 33(3), 442-449. doi.org/10.6018/analesps.33.3.271011.
[5] Ciolac, E. G., Guimarães, G. V., D´Avila, V. M., Bortolotto, L. A., Doria, E. L., & Bocchi, E. A. (2009). Acute effects of continuous and interval aerobic exercise on 24-h ambulatory blood pressure in long-term treated hypertensive patients. International Journal of Cardiology. 133(3), 381–387. doi.org/10.1016/j.ijcard.2008.02.005.
[6] Cunha, R. M., Costa, A. M., Silva, C. N. F., Póvoa, T. I. R., Pescatello, L. S., & Lehnen, A. M. (2018). Postexercise hypotension after aquatic exercise in older women with hypertension: A randomized crossover clinical trial. American Journal of Hypertension. 31(2), 247-252. doi.org/10.1093/ajh/hpx165.
[7] Cunha, R. M., Macedo, C. B., Araújo, S. F., Santos, J. C., Borges, V. S., Soares, A. A. Jr, ... & Pfrimer, L. M. (2012). Subacute blood pressure response in elderly hypertensive women after a water exercise session: a controlled clinical trial. High Blood Pressure & Cardiovascular Prevention. 19(4), 223-227. doi.org/10.1007/BF03297634.
[8] Cunha, R. M., Vilaça-Alves, J., Noleto, M. V., Silva, J. S., Costa, A. M., Silva, C. N., ... & Lehnen AM. (2017). Acute blood pressure response in hypertensive elderly women immediately after water aerobics exercise: A crossover study. Clinical and Experimental Hypertension. 39(1), 17-22. doi.org/10.1080/10641963.2016.1226891.
[9] Gómez-Jiménez, M., & López de Subijana-Hernández, C. (2016). Influence of Height on the Gait Patterns of Men and Women. Apunts. Educación Física y Deportes. 126, 30-36. doi.org/10.5672/apunts.2014-0983.es.(2016/4).126.03.
[10] González Robles, E. M., Pérez Aranda, J. R., & Alarcón Urbistondo, P. (2017). Main Causes Inducting Physical Sports Activity in Women. Apunts. Educación Física y Deportes. 129, 108-118. doi.org/10.5672/apunts.2014-0983.es.(2017/3).129.08.
[11] Granda Vera, J., Alemany Arrebola, I., & Aguilar García, N. (2018). Gender and its Relationship with the Practice of Physical Activity and Sporty. Apunts. Educación Física y Deportes. 132, 123-141. doi.org/10.5672/apunts.2014-0983.es.(2018/2).132.09.
[12] Guimarães, G. V., de Barros Cruz, L. G., Fernandes-Silva, M. M., Dorea, E. L., & Bocchi, E. A. (2014). Heated water-based exercise training reduces 24-hour ambulatory blood pressure levels in resistent hypertensive patients: A randomized controlled trial (HEx trial). International Journal of Cardiology. 172(2), 434-441. doi.org/10.1016/j.ijcard.2014.01.100.
[13] Herrod, P. J. J., Doleman, B., Blackwell, J. E. M., O’Boyle, F., Williams, J. P., Lund, J. N., & Phillips, B. E. (2018). Exercise and other nonpharmacological strategies to reduce blood pressure in older adults: a systematic review and meta-analysis. Journal of the American Society of Hypertension. 12(4), 248-267. doi.org/10.1016/j.jash.2018.01.008.
[14] Kruel, L. F. M., Posser, M. S., Alberton, C. L., Pinto, S. S., & Oliveira, A. S. (2009). Comparison of energy expenditure between continuous and interval water aerobic routines. International Journal of Aquatic Research and Education. 3(2), 186-196. doi.org/10.25035/ijare.03.02.09.
[15] MacDonald, J., MacDougall, J., & Hogben, C. (1999). The effects of exercise intensity on post exercise hypotension. Journal of Human Hypertension. 13(8), 527–531. doi.org/10.1038/sj.jhh.1000866.
[16] Mozaffarian, D., Benjamin, E.J., Go, A.S., Arnett, D.K., Blaha, M.J., Cushman, M., de Ferranti, S., Després, J.P., Fullerton, H.J., Howard, V.J., Huffman, M.D., Judd, S.E., Kissela, B.M., Lackland, D.T., Lichtman, J.H., Lisabeth, L.D., Liu, S., Mackey, R.H., Matchar, D.B., McGuire, D.K., Mohler, E.R., Moy, C.S., Muntner, P., Mussolino, M.E., Nasir, K., Neumar, R.W., Nichol, G., Palaniappan, L., Pandey, D.K., Reeves, M.J., Rodriguez, C.J., Sorlie, P.D., Stein, J., Towfighi, A., Turan, T.N., Virani, S.S., Willey, J.Z., Woo, D., Yeh, R.W., Turner, M.B.; American Heart Association Statistics Committee & Stroke Statistics Subcommittee. (2015). Heart Disease and Stroke Statistics-2015 Update: a report from the American Heart Association. Circulation. 131(4), e29-322. doi.org/10.1161/CIR.0000000000000152.
[17] Pescatello, L. S., Franklin, B. A., Fagard, R., Farquhar, W. B., Kelley, G. A., Ray, C. A., & American College of Sports Medicine (2004). American College of Sports Medicine position stand. Exercise and hypertension. Medicine and Science in Sports and Exercise. 36(3), 533–553. doi.org/10.1249/01.mss.0000115224.88514.3a.
[18] Pinto, S. S., Umpierre, D., Ferreira, H. K., Nunes, G. N., Ferrari, R., & Alberton, C. L. (2017). Postexercise hypotension during different water-based concurrent training intrasession sequences in young women. Journal of the American Society of Hypertension. 11(10), 653-659. doi.org/10.1016/j.jash.2017.08.002.
[19] Pontes-Junior, F.L., Bacurau, R.F., Moraes, M.R., Navarro, F., Casarini, D.E., Pesquero, J.L., Pesquero, J.B., Araújo, R.C. & Piçarro, I.C. (2008). Kallikrein Kinin system activation in post-exercise hypotension in water running of hypertensive volunteers. International Immunopharmacology. 8(2), 261-266. doi.org/10.1016/j.intimp.2007.09.001.
[20] Rim, H., Yun, Y.M., Lee, K.M., Kwak, J.T., Ahn, D.W., Choi, J.K., Kim, K.R., Joh, Y.D., Kim, J.Y. & Park, Y.S. (1997). Effect of physical exercise on renal response to head-out water immersion. Applied Human Science. 16(1), 35-43. doi.org/10.2114/jpa.16.35.
[21] Rodriguez, D., Silva, V., Prestes, J., Rica, R. L., Serra, A. J., Bocalini, D. S., & Pontes, F. L. Jr. (2011). Hypotensive response after water-walking and land-walking exercise sessions in healthy trained and untrained women. International Journal of General Medicine. 4, 549-554. doi.org/10.2147/IJGM.S23094.
[22] Sosner, P., Gayda, M., Dupuy, O., Garzon, M., Lemasson, C., Gremeaux, V., Lalongé, J., Gonzales, M., Hayami, D., Juneau, M., Nigam, A., & Bosquet, L. (2016). Ambulatory blood pressure reduction following high-intensity interval exercise performed in water or dryland condition. Journal of the American Society of Hypertension. 10(5), 420-428. doi.org/10.1016/j.jash.2016.02.011.
[23] Srámek, P., Simecková, M., Janski, L., Savlíková, J., & Vybíral, S. (2000). Human Physiological responses to immersion into water of different temperatures. European Journal of Applied Physiology. 81(5), 436-442. doi.org/10.1007/s004210050065.
[24] Terblanche, E., & Millen, A. M. (2012). The magnitude and duration of post-exercise hypotension after land and water exercises. European Journal of Applied Physiology. 112(12), 4111-4118. doi.org/10.1007/s00421-012-2398-5.
[25] Whelton, P.K., Carey, R.M., Aronow, W.S., Casey Jr, D.E., Collins, K.J., Dennison Himmelfarb, C., DePalma, S.M., Gidding, S., Jamerson, K.A., Jones, D.W., MacLaughlin, E.J., Muntner, P., Ovbiagele, B., Smith Jr, S.C., Spencer. C.C., Stafford, R.S., Taler, S.J., Thomas, R.J., Williams Sr, K.A., Williamson, J.D. & Wright Jr, J.T. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 138(17), e426-e483. doi.org/10.1161/CIR.0000000000000597.
ISSN: 2014-0983
Received: June 22, 2020
Accepted: January 14, 2021
Published: April 01, 2021
Editor: © Generalitat de Catalunya Departament de la Presidència Institut Nacional d’Educació Física de Catalunya (INEFC)
© Copyright Generalitat de Catalunya (INEFC). This article is available from url https://www.revista-apunts.com/. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/deed.en



