Validation of Oxygen Consumption Prediction Equations and New Formulas for Interval Training
*Corresponding author: Bruno Bazuelo-Ruiz bruno.bazuelo@uv.es
Cite this article
Bazuelo-Ruiz, B., De Rosario, H., & Durá-Gil, J.V., (2021). Validation of oxygen consumption prediction equations and new formulas for interval training. Apunts. Educación Física y Deportes, 143, 9-16. https://doi.org/10.5672/apunts.2014-0983.es.(2021/1).143.02
Abstract
Objectives. Our aims were to determine whether there is any significant difference between the measured and estimated energy expenditure for the most commonly used prediction equations in the literature, and to develop a new specific prediction equation for aerobic interval training with a broader cross-section of the population in terms of age, fitness and body mass index (BMI).
Methods.Twenty healthy participants were recruited for this study. Two groups of ten people were established depending on their BMI. The low BMI group ranged between 19 and 22, and the high BMI group between 26 and 29. The test protocol consisted of 12 individualized intensities, 6 walking and 6 running speeds on a treadmill, measuring both heart rate and energy expenditure. The rest time between intervals ranged between 1 and 2 minutes
Main results. The measured oxygen consumption was found to be significantly different from those predicted by the walking and running equations selected from the literature. The Léger equation was the best of the tested equations to estimate oxygen consumption for walking and the ACSM formula was the best for running. However, neither was found to be very accurate.
Conclusions. The prediction equations selected from the literature in this study were not accurate enough to estimate oxygen consumption during aerobic interval training. We propose four new formulas to improve the estimation of the metabolic cost in interval activities in a population with wider characteristics than those found in the literature.
Introduction
Estimating metabolic cost during exercise has been studied for a long time due its relevance in individualized exercise prescription. More precise knowledge about individual energy expenditure (EE) is useful for the medical community, sports trainers and individual patients. Walking and running are the most widely recommended physical activities in populations aiming to improve their quality of life. In fact, most EE prediction equations focus on walking and running modalities. Within these modalities, it is still unknown what key factors – such as volume, frequency, intensity and density – are most suitable for each case. Continuous moderate-intensity exercise (CMIE) has been traditionally prescribed by doctors and sports trainers. However, new types of exercise, like aerobic interval training (AIT), have gained popularity because of their adherence to exercise (Currie et al., 2013) and enhanced benefits compared to CMIE (Hwang et al., 2011; Warburton et al., 2005). Interval exercises can be defined as repeated short bouts of work phases followed by short recovery phases. The main benefits detailed in previous studies include improvements in endothelial and mitochondrial function (Wisløff et al., 2007), functional capacity gains (Daussin et al., 2007; Helgerud et al., 2007) and prevention of cardiovascular diseases (Kemi & Wisloff, 2010). These improvements can all result in a better quality of life (Nilsson et al., 2008) and many people can benefit from this kind of exercise, whether healthy participants (Tsukamoto et al., 2016) or patients with heart disease (Rognmo et al., 2004).
The direct determination of EE is expensive, time-consuming and subject to laboratory conditions. On the other hand, a valid alternative is oxygen consumption estimation from prediction equations found in the literature. Most variables measured for this estimation were acceleration parameters (Bouten et al., 1994; Staudenmayer et al., 2009), heart rate (HR) signals (Keytel et al., 2005; Pettitt et al., 2007) or spatio-temporal parameters (Glass et al., 2007; Hall et al., 2004; Loftin et al., 2010). However, a disadvantage of these equations is that the population used in most investigations was very similar, typically young healthy participants. Moreover, all equations were designed for steady-state submaximal exercise.
Therefore, our aims were (i) to determine whether there is any significant difference between the measured and estimated energy expenditure (EE) for the most commonly used prediction equations in the literature, and (ii) to develop a new specific prediction equation for aerobic interval training with a broader cross-section of the population in terms of age, fitness and body mass index (BMI).
Methodology
Participants
Twenty healthy participants (10 males and 10 females) were recruited for this investigation. Two groups of ten people were established depending on their body mass index (BMI). The characteristics of the study participants were the following: Low BMI (5 males and 5 females): age 30 ± 9.2 years; body mass 59.17 ± 8.71 kg; height 1.71 ± .13 m; BMI 20.17±.81; High BMI (5 males and 5 females): age 40.2 ± 9.3 years; body mass 78.86 ± 13.63 kg; height 1.67 ± .14 m; BMI 28.17 ± 1.17. The low BMI group ranged between 19 and 22 and the high BMI group between 26 to 29. All participants reported that they were free from any cardiac disease or injury that could limit their ability to complete the test. Participants refrained from strenuous exercise for a minimum of 24 hours and refrained from caffeine consumption for at least 6 hours before each testing session. The study protocol adhered to the tenets of the Declaration of Helsinki and received the Ethics Committee approval of the Polytechnic University of Valencia. All participants gave their informed, written consent.
Procedure
The test protocol consisted of 12 individualized intensities, 6 walking and 6 running speeds. These were established as the participants warmed up according to their individual fitness levels. Regarding the walking and running modalities, participants had to report three speeds. For the walking modality, the first was a comfortable walking speed that participants were used to while walking normally, while the second was a speed at which they could walk and run slowly. From this range, it was equally subdivided in 6 parts to get the 6 walking speeds. The maximum walking speed was selected as the lowest running speed (light jogging). The maximum running speed corresponded to the speed at which participants could maintain at least 4 minutes without reaching visible signs of high levels of fatigue. From the lowest and maximum running speeds, this range was equally subdivided to get the 6 running speeds. Having established their individual speeds, all participants performed 12 different speeds in a randomized order. The reason to establish this number of repetitions or speeds was to analyse if prediction equations worked correctly in different intensities of walking and running, not just one walking or running speed. Each speed lasted 3 minutes and between there was a rest time of 1 minute after walking speeds and 2 minutes after running speeds. Three minutes was enough time to measure stable oxygen consumption (Nieman, 2010). From this time, the last two minutes for each speed were taken into account for energy consumption analysis (Nieman, 2010). Before the warm-up period, the resting heart rate (HRrest) and energy expenditure were measured over a period of 5 minutes in a sitting position.
Material and Instruments
The tests were performed on a calibrated treadmill (HP Cosmos, Mercury, Germany) with a 1% treadmill grade (Jones and Doust, 1996). HR signals were measured by a nECG MINDER (Nuubo, Spain), which was placed on the participant’s chest. Energy expenditure was measured by indirect calorimetry, utilizing open circuit spirometry of the Cosmed K4b2 metabolic analyser (Rome, Italy). The gas analyser was calibrated every morning before the commencement of the tests.
Data analysis
Many formulas have been used in the literature to calculate oxygen consumption. We selected the following prediction equations because they are the most frequently used by physiologists and researchers in their studies.
Walking:
EQ1 (Glass et al., 2007): VO2 (ml/kg/min) = .1 * S 1.8 * S * fractional grade + 3.5; where S is the speed in m/min; fractional grade is in decimal form, 5% grade is.05.
EQ2 (van der Walt & Wyndham, 1973): VO2 (L/min): .00599 * M + .000366 * M * V2; where M: body mass (kg), V: velocity (m/s).
EQ3 (Léger & Mercier, 1984): VO2 (mL/kg/min) = 2.209 + 3.1633 * V; donde V where V: walking speed in km/h.
EQ4 (Pettitt et al., 2007): METS = 6 * HRindex - 5;
HRindex = HRabsolute / HRrest
EQ5 (Keytel et al., 2005): EE (kJ/min) = gender * (-55.0969 + .6309 * heart rate + .1988 * weight + .2017 * age) + (1 - gender) * (-20.4022 + .4472 * heart rate – .1263 * weight + .074 * age); where Male = 1, Female = 0; 1 l O2/min = 20 kJ/min.
Running:
EQ6 (Glass et al., 2007): VO2 (ml/kg/min) = .2
* S + .9 * S * fractional grade + 3.5; where S is the speed in m/min; fractional grade is in decimal form, 5% grade is .05.
EQ7 (van der Walt & Wyndham, 1973): VO2 (L/min): -.419 + .03257 * M + .000117 * M * V2; where M: body mass (kg), V: velocity (m/s).
EQ8 (Léger & Mercier, 1984): VO2 (mL/kg/min) = 2.209 + 3.1633 * V; where V: running speed in km/h.
EQ9 (Pettitt et al., 2007): METS = 6 * HRindex – 5; HRindex = HRabsolute / HRrest; 1MET = 3.5 mL/kg/min.
EQ10 (Keytel et al., 2005): EE (kJ/min) = gender * (-55.0969 + .6309 * heart rate + .1988 * weight + .2017 * age) + (1 – gender) * (-20.4022 + .4472 * heart rate - .1263 * weight + .074 * age); where Male=1, Female=0; 1 l O2/ min = 20 kJ/min.
Before starting the statistical analysis, the results obtained from every equation were converted to ml/Kg/min, in order to unify and be able to compare between them. A paired t-test was performed to calculate the difference and significance within the measured and estimated VO2 values for each equation used. In order to calculate the magnitude of the error, the absolute values of the differences between estimated and measured values were also taken into account. Statistical significance was set at the .05 level. Different models for walking and running through a multiple linear regression analysis were then generated to improve the accuracy for this population and type of physical activity (interval training). The models were adjusted by HRindex, BMI, gender, speed and age. HRindex is the mean absolute HR divided by the HRrest.
Results
The speed range (mean ± SD) for the walking modality was .71 ± .12 m·s-1 to 1.74 ± .31 m·s-1 and 1.74 ± .31 m·s-1 to 2.55 ± .67 m·s-1 for the running modality was.
The measured VO2 was found to be significantly different (p < .05) from all walking and running prediction equations used for this analysis. For walking, Table I showed that EQ1, EQ2 and EQ4 underestimate the measured VO2, and EQ3 and EQ5 overestimate the measured VO2. For running, EQ6, EQ7, EQ8 and EQ9 underestimate the measured VO2 and EQ10 overestimates the measured VO2.
We analysed the independent variables that affect the walking and running models and propose two models for each, depending on whether or not the HR signal is used as an independent variable. The first model obtained was used with all variables (HRindex, BMI, gender, speed and age) but BMI (low or high) and gender (male or female) were not significant (p > .05), therefore, these variables were excluded in the final models. Table II shows the model coefficients for the walking modality using HRindex as an independent variable, while Table III shows the model for the walking modality without HRindex. Table IV and Table V show the model coefficients for running with and without HRindex, respectively.
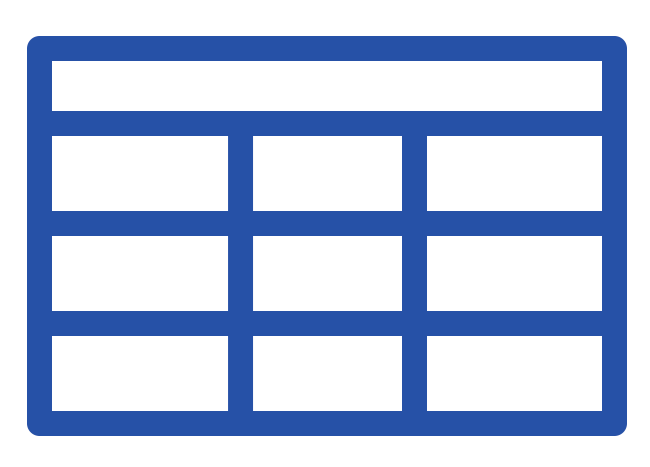
Table 1
Measured and estimated VO2 values and difference between measured and estimated for walking (EQ1-EQ5) and running (EQ6-EQ10). Values expressed in mL·kg·min-1 (mean±SD).
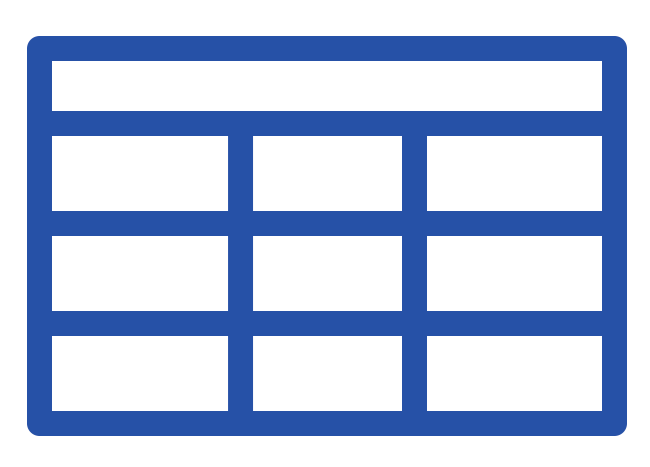
Table 2
Coefficients and significance for the multiple linear regression model adjusted by age, HRindex and walking speed.
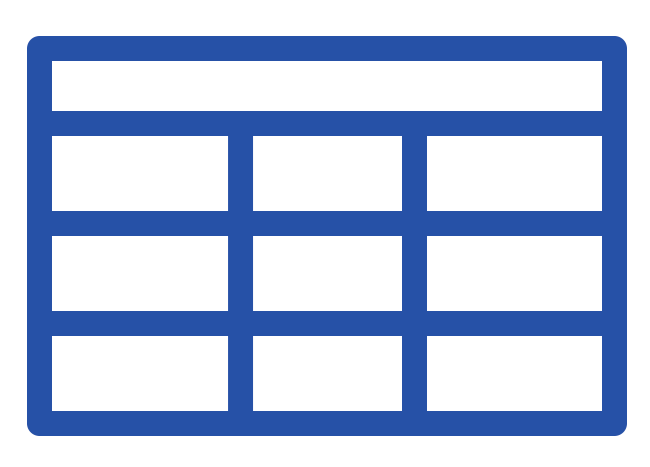
Table 3
Coefficients and significance for the multiple linear regression model adjusted by age and walking speed.
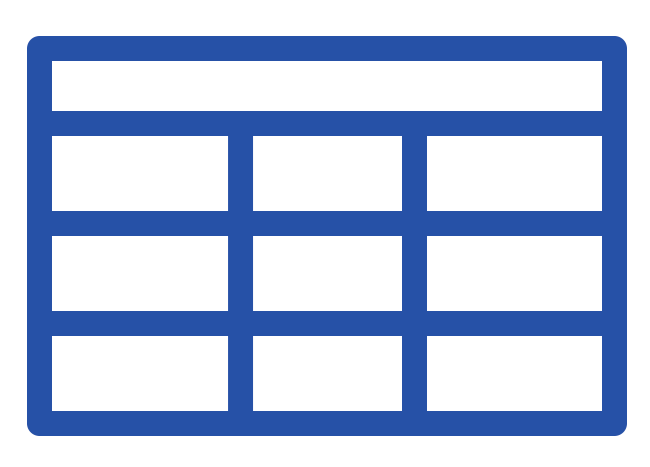
Table 4
Coefficients and significance for the multiple linear regression model adjusted by age, HRindex and running speed.
Table 5
Coefficients and significance for the multiple linear regression model adjusted by age and running speed.
The regression models generated allowed for a more accurate prediction equation for both walking and running for this population. Figure I shows that our prediction equations have a lower absolute error (mean ± SD) with respect to the measured VO2. The absolute differences of our prediction equations for running were 2.60 ± 2.47 mL·kg·min-1 and 2.79 ± 2.40 mL·kg·min-1 when HR signals are included and excluded, respectively. For walking, we improved to an even greater extent the estimation of VO2 with the absolute differences as 1.44±1.17 mL·kg·min-1 and 1.79 ± 1.52 mL·kg·min-1 when HR signals are included and excluded, respectively.
Discussion
This study focused on measuring oxygen consumption during aerobic interval training in a population with different energetic demands and BMI values. First, we compared the accuracy of the measured and estimated O2 consumption for AIT. Then, if this was found to be not accurate enough, we proposed four new formulas to improve the estimation of metabolic cost in interval activities in a population with more varied characteristics than previously found in the literature.
The sample used in most studies is young, healthy and of normal weight, with a BMI lower than 25 (Glass et al., 2007). The sample tested consisted of participants with different characteristics that had not been previously tested. The sample of Hall et al. (2004) was different. They recruited a total of 24 participants with a BMI ranging from 20 to 27.4; however the mean BMI for women and men was 22.37 and 23.64, respectively. Another difference with our study is the mean age, being 21.4 and 23.2 years for women and men respectively in their study. Otherwise, Loftin et al. (2010) developed a prediction equation for a population similar to our own but the EE estimation was for a given distance (1 mile) rather than for a given time or speed, which is usually used in interval training.

The specificity of the activity employed for measuring oxygen consumption in the training activity is relevant if accuracy is being sought. ACSM´s equations (Glass et al., 2007) are frequently used in the literature by physiologists and trainers, though they have some limitations. They were designed for steady-state exercises and are dependent upon speed range (.83 to 1.66 m·s-1 in the walking equation and greater than 2.22 m·s-1 in the running equation). There is therefore a gap missing for the 1.66 to 2.22 m·s-1 speed range. Moreover, some studies (Hall et al., 2004; Koutlianos et al., 2013; Loftin et al., 2010; Peterson et al., 2003) have cross-validated ACSM´s prediction equations and concluded that they are not capable of accurately predicting O2 consumption. This is due to the application of these formulas to different protocols or exercise modalities.
Weyand et al. (2013) found that the ACSM prediction equation for walking significantly underestimated the metabolic rate. Our results agreed with this study but indicated that EQ3 was the best of the tested equations to estimate O2 consumption in the walking modality and EQ6 was the best for the running modality. However, neither is accurate enough (p < .05) when compared with measured values. For running, the worst prediction equations were those using HR signals as input to estimate metabolic cost.
The EE in walking and running are different, being higher for the latter. We also determined that the EE in the running modality was higher than in the walking modality for the same absolute speed. Therefore, as noted in other investigations (Glass et al., 2007; van der Walt & Wyndham, 1973) it was necessary to design separate equations for walking and running.
To the best of our knowledge, there are no equations that can accurately predict O2 consumption for AIT in a population with different BMI values. Therefore, we developed two prediction equations for walking and two for running, including age (years), speed (in km/h) and HRindex(HRabsolute / HRrest):
Walking:
EQNew_W_HR (ml/kg/min) = 13.031 –.068 * Age + .586 * Speed2 + 2.088 * HRindex – 2.454 * Speed
EQNew_W (ml/kg/min) = 15.227 – .055 * Age + .603 * Speed2 - 2.425 * Speed
Running:
EQNew_R_HR (ml/kg/min) = 6.415 – .087 * Age + 3.051 * HRindex + 2.877 * Speed
EQNew_R (ml/kg/min) = 9.302 – .047 * Age + 3.107 * Speed
We found that the inclusion of HRindex to estimate VO2 consumption resulted in greater accuracy. However, for a given exercise intensity, as ambient temperature increases, HR also increases, with little or no corresponding increase in EE (Hebestreit & Bar-Or, 1998).
Conclusions
The prediction equations selected from the literature in this study were not accurate enough to estimate oxygen consumption during aerobic interval training. We propose four new formulas to improve the estimation of the metabolic cost in interval activities in a population with wider characteristics than those found in the literature. From a practical perspective, in real conditions the equations should be used with caution. Additionally, the proposed equations can be used to estimate oxygen consumption in aerobic interval activities, such as walking or running, although we caution that these formulas have not been cross-validated. Further studies should validate them.
References
[1] Bouten, C. V., Westerterp, K. R., Verduin, M., & Janssen, J. D. (1994). Assessment of energy expenditure for physical activity using a triaxial accelerometer. Medicine and Science in Sports and Exercise, 26(12), 1516–1523. doi.org/10.1249/00005768-199412000-00016
[2] Currie, K. D., Dubberley, J. B., McKelvie, R. S., & MacDonald, M. J. (2013). Low-volume, high-intensity interval training in patients with CAD. Medicine and Science in Sports and Exercise, 45(8), 1436–1442. doi.org/10.1249/MSS.0b013e31828bbbd4
[3] Daussin, F. N., Ponsot, E., Dufour, S. P., Lonsdorfer-Wolf, E., Doutreleau, S., Geny, B., Piquard, F., & Richard, R. (2007). Improvement of VO2max by cardiac output and oxygen extraction adaptation during intermittent versus continuous endurance training. European Journal of Applied Physiology, 101(3), 377–383. doi.org/10.1007/s00421-007-0499-3
[4] Glass, S., Dwyer, G. B., & Medicine, A. C. of S. (2007). ACSM’s Metabolic Calculations Handbook. Lippincott Williams & Wilkins.
[5] Hall, C., Figueroa, A., Fernhall, B., & Kanaley, J. A. (2004). Energy expenditure of walking and running: comparison with prediction equations. Medicine and Science in Sports and Exercise, 36(12), 2128–2134. doi.org/10.1249/01.mss.0000147584.87788.0e
[6] Hebestreit, H., & Bar-Or, O. (1998). Influence of climate on heart rate in children: comparison between intermittent and continuous exercise. European Journal of Applied Physiology and Occupational Physiology, 78(1), 7–12.
[7] Helgerud, J., Høydal, K., Wang, E., Karlsen, T., Berg, P., Bjerkaas, M., Simonsen, T., Helgesen, C., Hjorth, N., Bach, R., & Hoff, J. (2007). Aerobic high-intensity intervals improve VO2max more than moderate training. Medicine and Science in Sports and Exercise, 39(4), 665–671. doi.org/10.1249/mss.0b013e3180304570
[8] Hwang, C.-L., Wu, Y.-T., & Chou, C.-H. (2011). Effect of aerobic interval training on exercise capacity and metabolic risk factors in people with cardiometabolic disorders: a meta-analysis. Journal of Cardiopulmonary Rehabilitation and Prevention, 31(6), 378–385. doi.org/10.1097/HCR.0b013e31822f16cb
[9] Jones, A. M., & Doust, J. H. (1996). A 1% treadmill grade most accurately reflects the energetic cost of outdoor running. Journal of Sports Sciences, 14(4), 321–327. doi.org/10.1080/02640419608727717
[10] Kemi, O. J., & Wisloff, U. (2010). High-intensity aerobic exercise training improves the heart in health and disease. Journal of Cardiopulmonary Rehabilitation and Prevention, 30(1), 2–11. doi.org/10.1097/HCR.0b013e3181c56b89
[11] Keytel, L. R., Goedecke, J. H., Noakes, T. D., Hiiloskorpi, H., Laukkanen, R., van der Merwe, L., & Lambert, E. V. (2005). Prediction of energy expenditure from heart rate monitoring during submaximal exercise. Journal of Sports Sciences, 23(3), 289–297. doi.org/10.1080/02640410470001730089
[12] Koutlianos, N., Dimitros, E., Metaxas, T., Cansiz, M., Deligiannis, A., & Kouidi, E. (2013). Indirect estimation of VO2max in athletes by ACSM’s equation: valid or not? Hippokratia, 17(2), 136–140.
[13] Léger, L., & Mercier, D. (1984). Gross energy cost of horizontal treadmill and track running. Sports Medicine (Auckland, N.Z.), 1(4), 270–277.
[14] Loftin, M., Waddell, D. E., Robinson, J. H., & Owens, S. G. (2010). Comparison of energy expenditure to walk or run a mile in adult normal weight and overweight men and women. Journal of Strength and Conditioning Research, 24(10), 2794–2798. doi.org/10.1519/JSC.0b013e3181cc26cd
[15] Nieman, D. (2010). Exercise Testing and Prescription: A Health-Related Approach (7.ª edición). McGraw-Hill Education.
[16] Nilsson, B. B., Westheim, A., & Risberg, M. A. (2008). Effects of group-based high-intensity aerobic interval training in patients with chronic heart failure. The American Journal of Cardiology, 102(10), 1361–1365. doi.org/10.1016/j.amjcard.2008.07.016
[17] Peterson, M. J., Pieper, C. F., & Morey, M. C. (2003). Accuracy of VO2(max) prediction equations in older adults. Medicine and Science in Sports and Exercise, 35(1), 145–149. doi.org/10.1097/00005768-200301000-00022
[18] Pettitt, R. W., Pettitt, C. D., Cabrera, C. A., & Murray, S. R. (2007). A theoretical method of using heart rate to estimate energy expenditure during exercise. International Journal of Sports Science & Coaching, 2(3), 319–327. doi.org/https://doi.org/10.1260/174795407782233146
[19] Rognmo, Ø., Hetland, E., Helgerud, J., Hoff, J., & Slørdahl, S. A. (2004). High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. European Journal of Cardiovascular Prevention and Rehabilitation: Official Journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology, 11(3), 216–222. doi.org/10.1097/01.hjr.0000131677.96762.0c
[20] Staudenmayer, J., Pober, D., Crouter, S., Bassett, D., & Freedson, P. (2009). An artificial neural network to estimate physical activity energy expenditure and identify physical activity type from an accelerometer. Journal of Applied Physiology (Bethesda, Md.: 1985), 107(4), 1300–1307. doi.org/10.1152/japplphysiol.00465.2009
[21] Tsukamoto, H., Suga, T., Takenaka, S., Tanaka, D., Takeuchi, T., Hamaoka, T., Isaka, T., Ogoh, S., & Hashimoto, T. (2016). Repeated high-intensity interval exercise shortens the positive effect on executive function during post-exercise recovery in healthy young males. Physiology & Behavior, 160, 26–34. doi.org/10.1016/j.physbeh.2016.03.029
[22] Van der Walt, W. H., & Wyndham, C. H. (1973). An equation for prediction of energy expenditure of walking and running. Journal of Applied Physiology, 34(5), 559–563. doi.org/10.1152/jappl.1973.34.5.559
[23] Warburton, D. E. R., McKenzie, D. C., Haykowsky, M. J., Taylor, A., Shoemaker, P., Ignaszewski, A. P., & Chan, S. Y. (2005). Effectiveness of high-intensity interval training for the rehabilitation of patients with coronary artery disease. The American Journal of Cardiology, 95(9), 1080–1084. doi.org/10.1016/j.amjcard.2004.12.063
[24] Weyand, P. G., Smith, B. R., Schultz, N. S., Ludlow, L. W., Puyau, M. R., & Butte, N. F. (2013). Predicting metabolic rate across walking speed: one fit for all body sizes? Journal of Applied Physiology (Bethesda, Md.: 1985), 115(9), 1332–1342. doi.org/10.1152/japplphysiol.01333.2012
[25] Wisløff, U., Støylen, A., Loennechen, J. P., Bruvold, M., Rognmo, Ø., Haram, P. M., Tjønna, A. E., Helgerud, J., Slørdahl, S. A., Lee, S. J., Videm, V., Bye, A., Smith, G. L., Najjar, S. M., Ellingsen, Ø., & Skjaerpe, T. (2007). Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation, 115(24), 3086–3094. doi.org/10.1161/CIRCULATIONAHA.106.675041
ISSN: 2014-0983
Received: 5 February 2020
Accepted: 8 July 2020
Published: 1 January 2021
Editor: © Generalitat de Catalunya Departament de la Presidència Institut Nacional d’Educació Física de Catalunya (INEFC)
© Copyright Generalitat de Catalunya (INEFC). This article is available from url https://www.revista-apunts.com/. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/deed.en


